Suicide is a leading cause of maternal mortality during pregnancy and the year after birth (the perinatal period). While maternal suicide is a relatively rare event, with an estimated prevalence of 1.6 to 4.5 per 100,000 live births in the United States, the impact of maternal suicide is profound and long-lasting.
Suicide attempt during pregnancy and the postpartum period is far more common. The prevalence of perinatal suicide attempt in the US is about 0.13%, or 130 per 100,000 live births, based on large statewide hospital and emergency department data. Most suicide attempts occur during the postpartum period rather than during pregnancy.
Suicide attempt in the perinatal period is distressing in its own right, but suicide attempt is also an important predictor of completed suicide. Thus, by understanding factors that contribute to suicide attempt, we may be able to understand perinatal suicide and identify women at greatest risk.
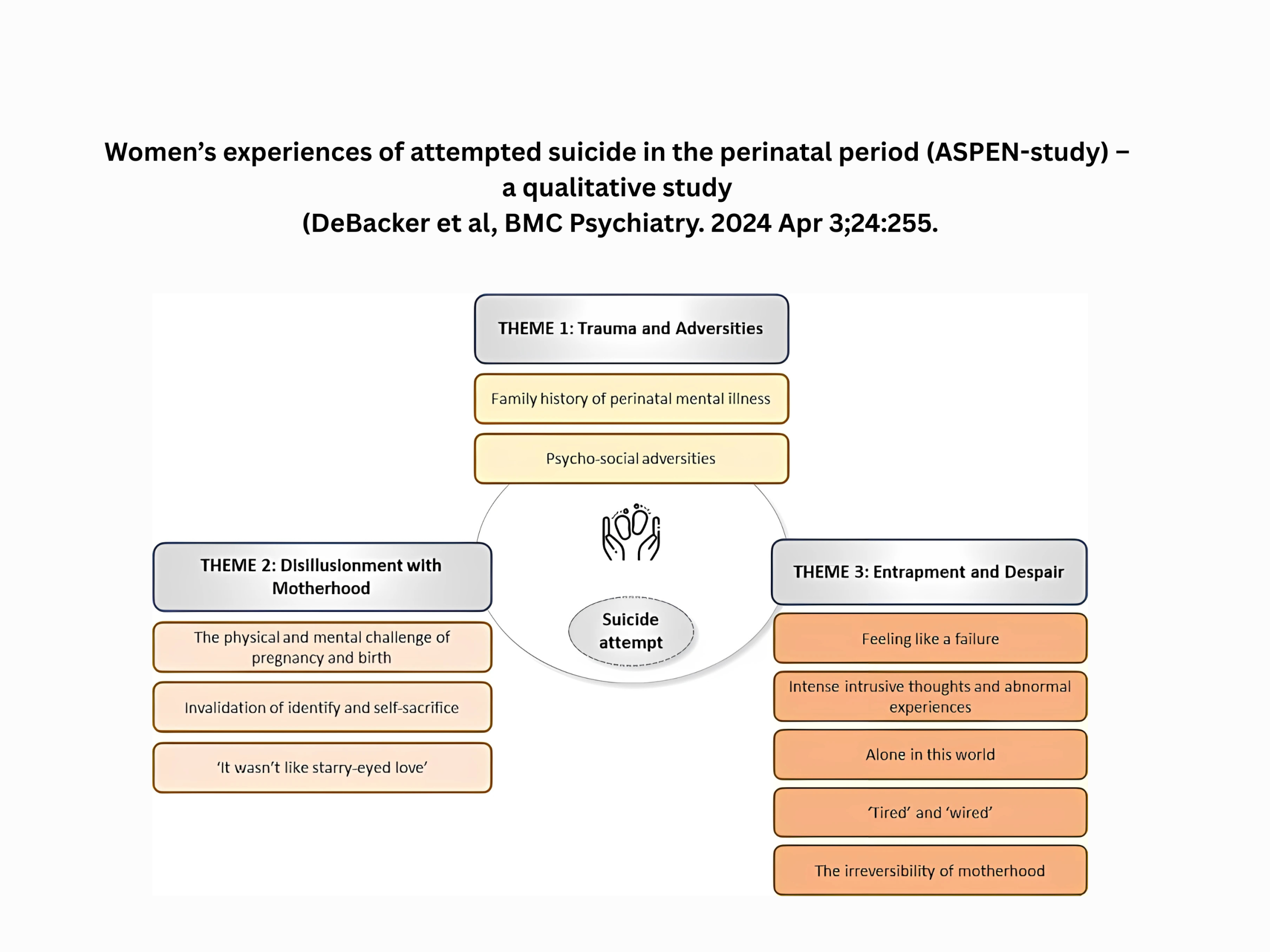
In this qualitative study, iterative feedback from a group of women with lived experience of perinatal mental illness and mental health providers was used to develop areas of exploration. The researchers recruited women (N = 11) in the United Kingdom who had self-reported having made a suicide attempt (within the past 10 years) during pregnancy or the postpartum period. Interviews were conducted virtually, recorded and transcribed. Thematic Analysis was used to develop themes and subthemes reflecting the women’s experiences. Three key themes contributing to perinatal suicide attempt were identified.
Trauma and Adversities
The theme of trauma and adversities reflects the significant vulnerabilities that all participants brought into the perinatal period. Nearly all respondents reported significant traumatic life events prior to pregnancy, often involving fractured or dysfunctional relationships, domestic abuse, and the chronic effects of unresolved grief or previous mental health challenges.
Some participants had suffered traumatic birth experiences in a prior pregnancy which shaped expectations and anxieties about subsequent pregnancies. In many cases, these psychosocial adversities were compounded by inadequate recognition or support from healthcare professionals.
Disillusionment with Motherhood
The theme of disillusionment with motherhood captures the profound gap between expectations of pregnancy, childbirth, and motherhood and the reality of these experiences. The study powerfully illustrates how participants’ hopes, as well as societal ideals, such as the supposed joy and “glow” of pregnancy, or the instant bond with a newborn, were often replaced by overwhelming physical and emotional challenges. Many women experienced severe illness, persistent pain from birth injuries, or a traumatic birth experience that contributed to feelings of alienation and a loss of control over their bodies.
Participants also described a deep sense of invalidation from healthcare providers, who focused solely on the baby’s wellbeing and neglected mothers’ emotional needs. This loss of identity was exacerbated by pressure to “perform” motherhood perfectly, driving exhaustion and self-sacrifice at the expense of their own wellbeing. An important subtheme was the inability to immediately bond with the baby, a perceived failure that resulted in feelings of guilt and shame and a persistent sense of detachment.
Entrapment and Despair
The final theme, entrapment and despair, reflects how cumulative stressors can culminate in overwhelming feelings of hopelessness, failure, and loss of control. Many women reported distressing, intrusive thoughts, and several reported psychotic experiences, including delusional thoughts and auditory hallucinations. These experiences were described as unexpected and deeply distressing and eroded mothers’ mental resilience and sense of safety. The inability to share these thoughts and experiences with others further exacerbated mothers’ sense of social isolation.
Sleep deprivation was nearly universal and played a critical role, with participants feeling persistently exhausted but trapped in a state of chronic hyperarousal or restlessness (“tired and wired”). Many described existential despair over the irreversibility of motherhood, feeling permanently “stuck” and powerless to revert to life before parenting. The baby was viewed paradoxically as both a cause of anguish and the sole reason to keep going on, deepening their internal conflict and sense of isolation. With mounting stress and little avenue for respite, feelings of entrapment grew so intense that suicide was perceived as the only escape from an intensely painful and unresolvable situation.
Clinical Implications
To date, research on perinatal suicide has predominantly relied on reviews of case notes, retrospective cohort studies, and investigations focusing on suicidal ideation, often leaving the context of actual suicide attempts underexplored. The novel qualitative study from De Backer and colleagues provides critical insights into the lived experiences of women who attempted suicide during the perinatal period and deepens our understanding of the complex interplay of circumstances that give rise to suicidality in this population.
Rather than attributing suicidal behaviors to a single causative factor, the authors emphasize that suicidal behaviors typically emerge from an accumulation of multiple, co-occurring life events and stressors. These factors interact and compound, culminating in an overwhelming sense of hopelessness and despair, wherein suicide is perceived as the only option. The following diagram from the article shows how these factors often overlap and amplify each other.
Many of the themes and subthemes revealed here, including social isolation, disappointment and disillusionment, loss of identity, inadequate support, and dismissiveness among health care providers, are frequently expressed by new mothers, especially those struggling with postpartum depression. While suicide attempt and suicide occur infrequently in this population, It seems that what may contribute to the progression to suicidal behavior is the feeeling of entrapment, the perception that no alternative resolution to their suffering exists.
Importantly, several of the mothers reported psychotic symptoms, including delusions and auditory hallucinations, and three of the 11 women were diagnosed with a psychotic disorder. Although this study does not emphasize the importance of psychotic symptoms, previous studies have clearly documented a high risk of suicide in women with postpartum psychosis. Further research is needed to determine whether the same themes and subthemes contribute to risk of suicidal behavior in women with non-psychotic disorders compared to those with psychotic disorders.
At the present time, we have no interventions designed specifically to target and reduce suicidal ideation and behavior among pregnant and postpartum women. Standard clinical practice focuses on treating psychiatric symptoms, such as depression, anxiety, or psychosis, but whether this sufficiently reduces suicide risk is not known. A more nuanced understanding of the factors leading up to a suicide attempt could help refine support and early interventions for women at risk.